March is Endometriosis Awareness Month, and this March, we asked members of the BuzzFeed community to let us know what questions they had about endometriosis. Then, we spoke directly to world-renowned endometriosis surgeon, reproductive immunologist, and reproductive endocrinologist, Dr. Andrea Vidali (along with his surgical fellow, Dr. Melissa McHale), to get some answers to your questions. See below for the questions and the doctor's answers to follow!
BTW: if you're wondering, "what exactly is endometriosis?" you can find more on what exactly this disease is along with other information you should know about it here.

Without further ado, let's get into it!
1. "Why do so few endometriosis surgeons accept insurance? Is there anything we can do to make care more accessible and affordable for all? How do you think endometriosis care could be more equitable?"
2. "How common is endometriosis on the bladder? What are the signs that people can be aware of?"
Dr. Vidali and Dr. McHale: Studies show that endometriosis of the bladder occurs in up to 12% of patients with endometriosis. It is much more common in patients with deep infiltrating endometriosis (DIE), where studies show that 20–50% of patients with DIE have bladder or ureter involvement of endometriosis. Endometriosis on the bladder can cause symptoms that at times can be confused with recurrent UTI ( Urinary tract Infections) but that in reality are due to bladder spasm. More information on that study here.
3. "Are there any truly helpful treatments and/or suggestions for adenomyosis aside from a hysterectomy from someone who cannot handle hormonal birth control?"

4. "Is there a hormonal component to Endo and if so, how does it work? It seems like there's a lot of conflicting information out there."
Dr. Vidali and Dr. McHale: Endometriosis lesions have hormone receptors for estrogen and progesterone — which means that circulating levels of hormones can stimulate the endometriosis tissue. So as hormone levels rise during the cycle, the implants become more active, releasing increased prostaglandins and causing pain and inflammation. The level of hormonal receptors can vary in endometriotic lesions so there is great variability on how such lesions behave when exposed to both endogenous or exogenous hormones. However, hormonal medications cannot eliminate or reduce the presence of endometriosis lesions.
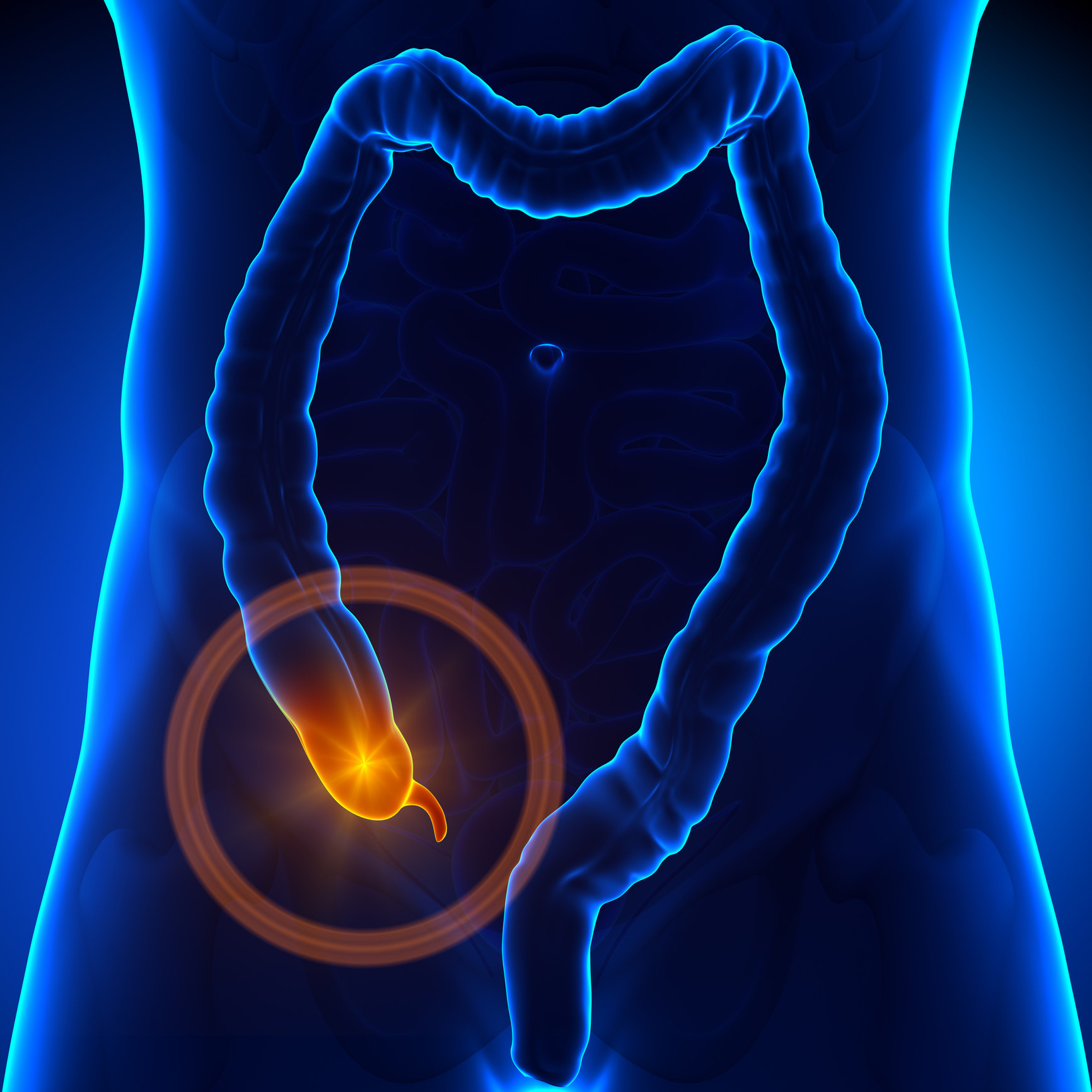
5. "Can you explain why surgeons may opt to remove the appendix during an excision surgery?"
6. "Is it true that endometriosis can only be accurately diagnosed through surgery?"
Dr. Vidali and Dr. McHale: In some patients this is the case — however, there are many patients in whom endometriosis can be diagnosed before surgery. For example, in patients with endometriomas (cysts on the ovaries filled with endometriosis) or nodules of endometriosis on the bowels or bladder, these can be seen very clearly on imaging such as MRI or ultrasound. These tend to be the more extensive or severe cases, but they can certainly be known prior to performing surgery and can help a patient know that their disease is extensive enough to require an expert surgeon. For patients without imaging findings that are suggestive of endometriosis, history should give a doctor a high index of suspicion that a patient may have endometriosis, but the diagnosis is ultimately only confirmed by laparoscopy.
7. "How long does proper excision surgery provide relief on average? What is the recurrence rate?"
8. "Is it possible to miss endometriosis during a laparoscopy?"
Dr. Vidali and Dr. McHale: Endometriosis is sometimes missed on laparoscopy when it is performed by a surgeon who does not see a high volume of endometriosis patients. However, there are many other drivers of pelvic pain, bladder symptoms, and bowel symptoms. So with continued symptoms and a previous negative laparoscopy, I would recommend a deep dive with a pelvic pain or endometriosis specialist on what is likely driving your symptoms — because other causes of pain may have other treatments that are effective.
9. "What exactly happens during a VATS for thoracic endometriosis?"

10. "I am curious about the impact of endometriosis on the Anti-Müllerian hormone and fertility — for example, I've heard endometriomas (a type of cyst that can form when endometrial tissue grows in the ovaries) can harm ovarian reserve. Is this true to your knowledge? What about just adhesions from endometriosis?"
Dr. Vidali and Dr. McHale: The Anti-Müllerian hormone or AMH is an important biomarker of ovarian reserve. Endometriosis certainly does have an impact on ovarian function. Endometriosis can cause decreased ovarian reserve and causes by directly damaging the ovary. This is particularly notable in patients with endometriomas. Immediately following surgery, the AMH can be even lower for a period of time, though we know that excision of endometriosis overall can have a positive effect on fertility. Timing of surgery endometriomas from the ovary is a decision to be made in conjunction with your fertility specialist: in some cases one should consider egg freezing prior to surgery. Endometriosis can certainly cause adhesions that can impair pregnancy, as they prevent normal transit of the egg to the fallopian tube and through it.
11. "Do you have tell-tale signs and/or symptoms that you would tell people to be aware of when it comes to endometriosis?"

12. "Can you talk about microscopic endometriosis? How common is this in your experience? What do we need to know about this?"
Dr. Vidali and Dr. McHale: Microscopic endometriosis falls into the category of what we often call “minimal disease”. In patients who have symptoms such as pelvic pain or infertility, performing excision of this disease can be very helpful in improving symptoms of pelvic pain and reducing inflammation in a way that improves fertility outcomes. A major problem that we encounter is lack of proper documentation of surgery: doctors do not take images at the time of the surgery. In our opinion, whenever possible it is important that you demand images from your surgery. This way, if there is a question about minimal endometriosis that could have been missed, this can be addressed without a repeat operation.
13. "Is endometriosis genetic?"
14. "If you have some form of ablation and the endometriosis grows back or continues to grow, can it be dangerous to your health if you don’t get it excised?"
Dr. Vidali and Dr. McHale: Ablation means thermal or laser destruction of endometriosis. It is less efficacious than excision, which means cutting out the endometriosis lesions. The risk of ablation surgery is that it is unlikely to completely resolve the problem and has a greater risk of recurrence.
15. "Does endometriosis resolve at menopause?"
16. "Are the stages that have previously been used for diagnosing endometriosis still useful? [E.g]: Stage 4 Endometriosis vs. Stage 1. Why or why not?"
Dr. Vidali and Dr. McHale: The old staging system developed by the ASRM (American Society for Reproductive Medicine) was developed with a major focus on fertility and does not correlate well with surgical complexity. There is a new staging system developed by the AAGL (American Association of Gynecologic Laparoscopists) and this system does correlate with surgical complexity and describes extent of disease. This system was just released last year, and so it is still being adopted into practice. You can find the app that is associated with this classification in the Apple store.
17. "There are some studies on Cannabinoids stopping the growth of endometriosis. Do you have any knowledge or thoughts around this?"
18. "Can endometriosis cause bladder incontinence?"
Dr. Vidali and Dr. McHale: Absolutely! However, there are multiple different things that can cause incontinence. Urge incontinence is reflective of bladder spasm which is absolutely triggered by endometriosis. The inflammation caused by endometriosis causes reactive bladder spasms that are manifested by a variety of symptoms, including frequent urination, waking up in the night to urinate, a feeling of incomplete emptying (feeling like you need to go again two minutes after you just went), and a feeling of significant discomfort when the bladder is full. Stress incontinence happens when a patient loses urine from laughing, coughing, sneezing or lifting — this is associated with things that compromise the strength of the pelvic floor, such as childbirth, connective tissue disorders, or other factors that are not endometriosis. Because there are so many nuances and treatments to bladder symptoms, it is important to discuss your specific symptoms with your doctor.
19. "I was told by an OBGYN that I should try to have a baby to cure my endometriosis, is that true?"
20. "Can you explain why a surgeon might recommend a hysterectomy when endometriosis is tissue outside of the uterus?"
Dr. Vidali and Dr. McHale: There are two different reasons that a doctor might recommend this — one being a good reason, and one being a bad reason. The good reason would be in a patient who does not desire future pregnancies and her doctor has reason to believe that there is a significant component of her pain caused by her uterus, removal of the uterus can be a good option. This especially applies to a patient with adenomyosis who does not desire pregnancy, or a patient with severe menstrual cramps who has previously undergone excision surgery without complete resolution of her pain. The bad reason would be if a doctor who recommends this to a patient in leu of excision surgery. Because menstrual symptoms are often prominent for patients with endometriosis, doctors who are not well versed in the treatment of endometriosis sometimes will recommend a hysterectomy in a misguided attempt to help their patients because it is a surgery that they are comfortable performing. Unfortunately, this is a major surgery that does not treat endometriosis and makes subsequent excision of endometriosis much more difficult to perform.
21. "In your experience, is it normal with endometriosis to get really bad cramps from penetration and sometimes also orgasms?"
22. And finally: "What made you both interested in becoming an endometriosis surgeon?"
Dr. Vidali: When I was doing my infertility fellowship at Columbia I was lucky to become part of a group of surgeons led by Dr. Harry Reich, a leader and an innovator in the area of endometriosis surgery. Dr. Reich was an inspiration for many. Along with Dr. Reich other doctors revolutionized the field. I would like to also mention the names of Dr. David Redwine, Dr. Camran Nezhat, Dr. CY Liu, and Dr. Liseotte Mettler. I believe surgery is a science, but also a craft, and mentorship is essential. This is why I decided to train some amazing doctors like Dr. McHale.
Dr. McHale: As a medical student, I was fortunate enough to do a rotation with an endometriosis specialist — I have never seen a doctor have such a profound impact on patients’ lives, and I decided to follow the same path! I love what I do — I love connecting with patients, I love pelvic surgery, and I love making a difference in patients’ lives — especially in a field where there is such a dire need for specialists.
