Hello, world! If you're reading this, you might already know that I have spent a good portion of my time here at BuzzFeed writing about what it has been like for me to live with endometriosis and other pelvic floor conditions for the better part of 15 years now. I am not alone in this. The statistics are that 1 in 10 women live with endometriosis (though not only women live with endometriosis — trans individuals and nonbinary individuals exist!), which means roughly ~200 million people worldwide.
March is Endometriosis Awareness Month, and this year, I wanted to compile a list of some of the information we do have about this disease. So in an effort to get the latest information — and because I genuinely might lose it if I see one more article suggesting that a hysterectomy is a cure for endometriosis — I compiled a list and then spoke with Dr. Matthew Siedhoff, Vice-Chair of Gynecology at Cedars-Sinai and excision surgeon, to get the latest information on this horrific disease.
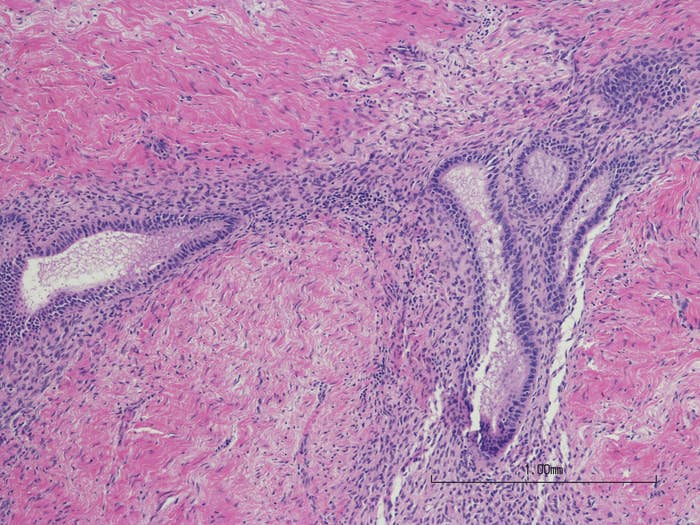
1. Endometriosis is not the lining of the uterus.
2. 1 in 10 people born with a uterus have endometriosis.
3. There are some common symptoms like pelvic pain, digestive issues, and painful sex. But there are also a whole other slew of symptoms that can be a sign of endometriosis.
4. It requires surgery to be definitively diagnosed with endometriosis, as endometriosis does not always appear on MRIs, CT scans, or ultrasounds.
5. And there is no such thing as "being too young to have endometriosis." Endometriosis does not have a minimum age requirement.
6. When talking about surgeries for endometriosis, there are two surgeries that are most commonly used in the treatment of endometriosis: ablation surgery and excision surgery. Excision surgery is currently considered the "gold-star" treatment for endometriosis.
7. And, according to Dr. Siedhoff, removing endometriosis during a proper excision surgery "can be as difficult or more difficult than surgery for cancer. It can be that aggressive in certain cases. So, finding someone who is experienced with the whole range of how endometriosis can present, I think, is a huge barrier to care."
8. But even if your pathology comes back as not having found endometriosis — unfortunately this doesn't mean that you don't have endometriosis, which is why symptoms are so important for doctors to pay attention to.
9. Pregnancy is not a cure for endometriosis.
10. And neither is menopause. Which brings me to discussing the most commonly prescribed pharmceutical drugs in the treatment of endometriosis: Leuprorelin (or Lupron Depot) and Orilissa (or Elagolix).

11. And a hysterectomy is not a cure for endometriosis because endometriosis, by definition, exists outside of the uterus. It is tissue that is *similar* to the lining of the uterus showing up other places in the body.
12. And as far as birth control goes — we really don't know whether or not this definitively stops the spread or growth of endometriosis.