Today was Medical Student Research Day. I went to two posters: one was about obesity, weight loss, and correlations with other adverse health outcomes, while the other was about ATV accidents and laws that can help to prevent them. The only problem was, there wasn't anyone at the obesity poster to do a presentation. Luckily, my friend Jessica was presenting the second poster.

1.
That's me standing at the first poster on obesity. I was intrigued by this poster for a few reasons. Before I came to medical school, I was a policy analyst at a Washington, D.C. think tank, where I studied social policies that prevent obesity at a population level. And, obesity (and associated metabolic conditions, like liver function, blood pressure, HgA1C, and blood glucose levels) have a pretty clear connection to our Foundations coursework.
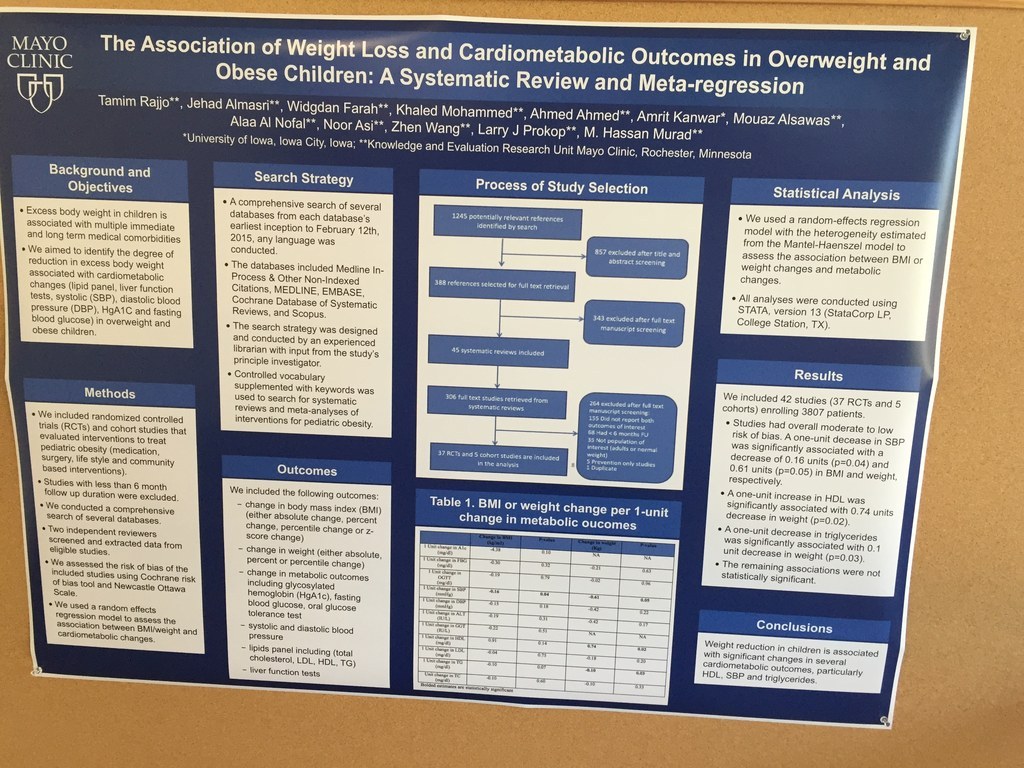
The poster presented here is from a meta-analyis of randomized controlled trials and cohort studies that evaluated interventions to treat pediatric obesity. The study aimed to identify the degree of reduction in excess body weight associated with cardiometabolic changes (lipid panel, liver function, systolic and diastolic blood pressure, HgA1C, and fasting blood glucose) in overweight and obese children. The authors found that significant changes in systolic blood pressure, triglycerides, and HDL were associated with a reduction in BMI and a decrease in weight. In Foundations, we've learned that excess glucose gets converted into glycogen, triglycerides, and fatty acids. Because we know that the body can only store a limited quantity of glycogen, the remaining excess energy will be converted into fat.
In my former life as a policy person, I sometimes forgot that obesity was biologically mediated. I chalked it up to a whole host of social and systematic problems, like neighborhood violence and poor walkability and government subsidies for corn (and thus corn-based unhealthy foods). This poster reminded me that there's a lot going on at a biochemical level that also needs to be explored and accounted for in policy making. And it left me with a lot of questions. Biochemically, when you lose weight, where is the excess fat going? What is the mechanism through which it leaves the body? And how does weight loss mediate changes in blood pressure and liver function and triglycerides on a biochemical level? I'm not going to answer these questions here, but I have some investigating to do.
2.
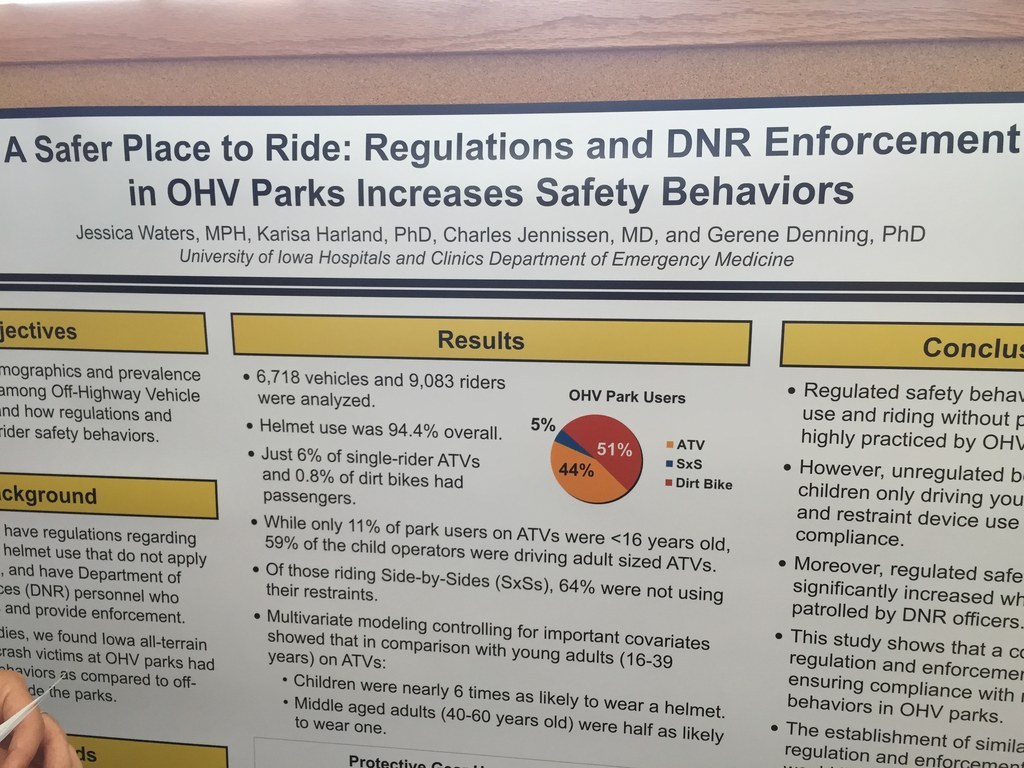
Next I visited Jessica's poster (because I needed to make sure I got full credit for actually talking to someone about their research and hearing a presentation). Jessica's poster is on ATV parks and safety measures. In Iowa's ATV parks, helmets and several other safety measures are mandated. For the most part, this study found that these laws are enforced and adhered to by park visitors. However, the rules in the parks don't apply once you've left the park, and few ATV riders wear protective gear or helmets outside of the parks. This leads to high rates of trauma injuries for ATV riders. This study found that children who ride adult sized ATVs make up 95% of the ATV related deaths. The authors concluded that legislation to mandate helmets and properly sized ATVs would dramatically reduce ATV related traumas.

This one is a bit harder to relate to Foundations, but it got me thinking: what happens to energetics in the cell when you experience trauma? We have learned about the normative pathways (and what happens when metabolism works perfectly as it should), as well as a few examples of how genetic mutations can cause things can go wrong in these pathways. But what's happening when something acute and VERY ABNORMAL happens? (Like when you crash your ATV and have head trauma.)
Let's say you're riding your ATV in a cornfield on your family's farm and you aren't wearing a helmet. You turn too quickly and you fall off and hit your head pretty bad. You're rushed to UIHC by helicopter, and later diagnosed with a traumatic brain injury (TBI). After hitting the ground, the cells in your brain are experiencing membrane disruption. They can't maintain ionic homeostasis, which leads to cytoxic oedema. Then you get an exocytotic release of glutamate, which exacerbates the disturbance of the trans-membrane ionic gradients. Additionally, calcium is accumulating in the mitochondria and inducing oxidative stress and impairing mitochondrial functioning. This leads to a generation of free radicals, highly reactive oxygen and nitrogen species, and leads to oxidative modification of proteins, lipids, and DNA. The result is that your inner mitochondrial membrane becomes more permeable, and when cytochrome c is released, you get capsase-dependent apoptosis and activation of poly-ADP ribose polymerase (a nuclear DNA repair enzyme that consumes NAD+, which is really needed to be doing glycolysis). The overall result is that you can't do glycolysis anymore, you get energy failure, the activation of apoptotic and necrotic pathways, and a traumatic brain injury. While this pathway isn't fully understood yet, according to a June 2015 literature review, there is the potential for your UIHC docts to target therapeutics (for your ATV-related TBI) to repairing the dysfunctional parts of your metabolic pathway (Jalloh et al., 2015).
3.
While I wrote this response, my new puppy has been very quietly resting in my lap. She's eight weeks old and her name is Callalily (Callie for short). She just had dinner an hour ago, so her doggy blood glucose levels are probably still pretty high right now. However, since she's resting, she doesn't really need to be using a lot of doggy ATP, so my guess is that she's making doggy glycogen to save some energy for later.

References
Jalloh, Ibrahim, et al. "Glucose metabolism following human traumatic brain injury: methods of assessment and pathophysiological findings." Metabolic brain disease 30.3 (2014): 615-632.

