A woman named Melissa Lima has gone viral for sharing how she found out she had breast implant illness, or BII (a term that refers to a variety of symptoms people can develop after getting breast implants).
She shared her story on TikTok, where it has received over 5 million views and thousands of comments. Melissa told BuzzFeed she got saline breast implants in 2002 and then had them replaced with smaller ones in 2005.
However, in 2010, she started experiencing a variety of really awful symptoms that included fatigue, brain fog, extreme anxiety and depression, weight gain, slow-healing cuts and scrapes, random rashes, sudden food allergies followed by intestinal issues, muscle and joint pain, and she developed an autoimmune disorder called Hashimoto's disease.
Doctors continuously performed blood tests on Melissa, but the diagnosis would always be the same: side effects from having Hashimoto's.
"Not a single doctor asked about my implants or associated any of my problems with them," she said.

So, on her own, Melissa decided to get her breast implants out after researching breast implant illness.

"I didn't know if removing them was going to 'cure' my problems. However, I was so sick, I decided I was going to get them taken out either way."

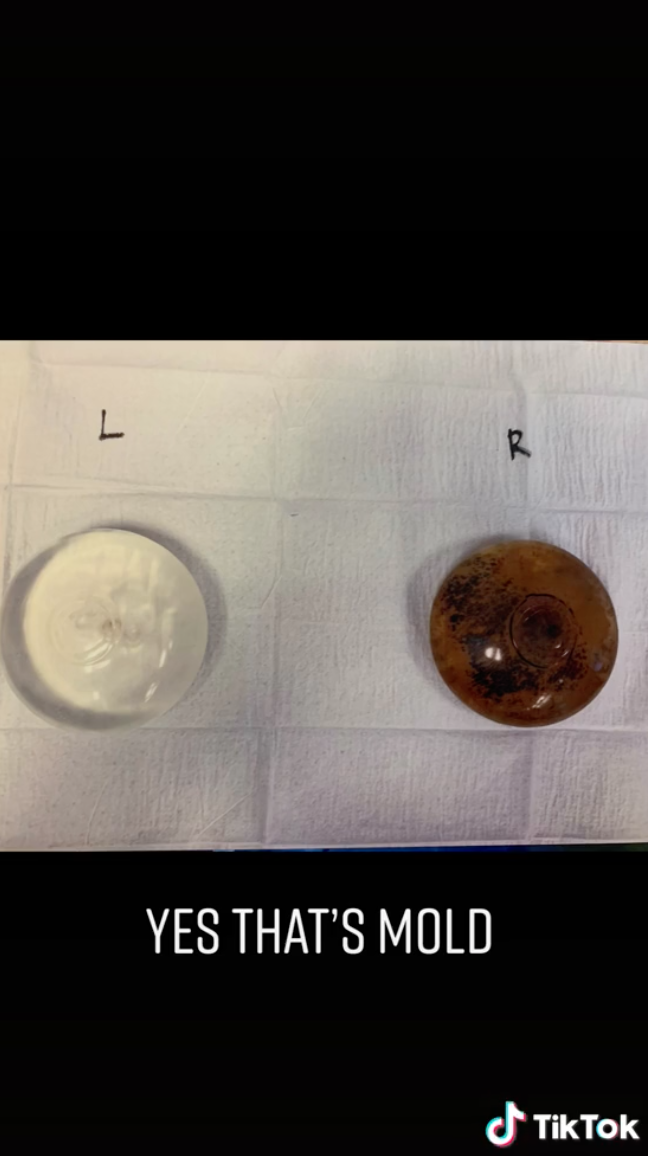
After the removal surgery in October of 2020, Melissa found out that one of her breast implants had mold.
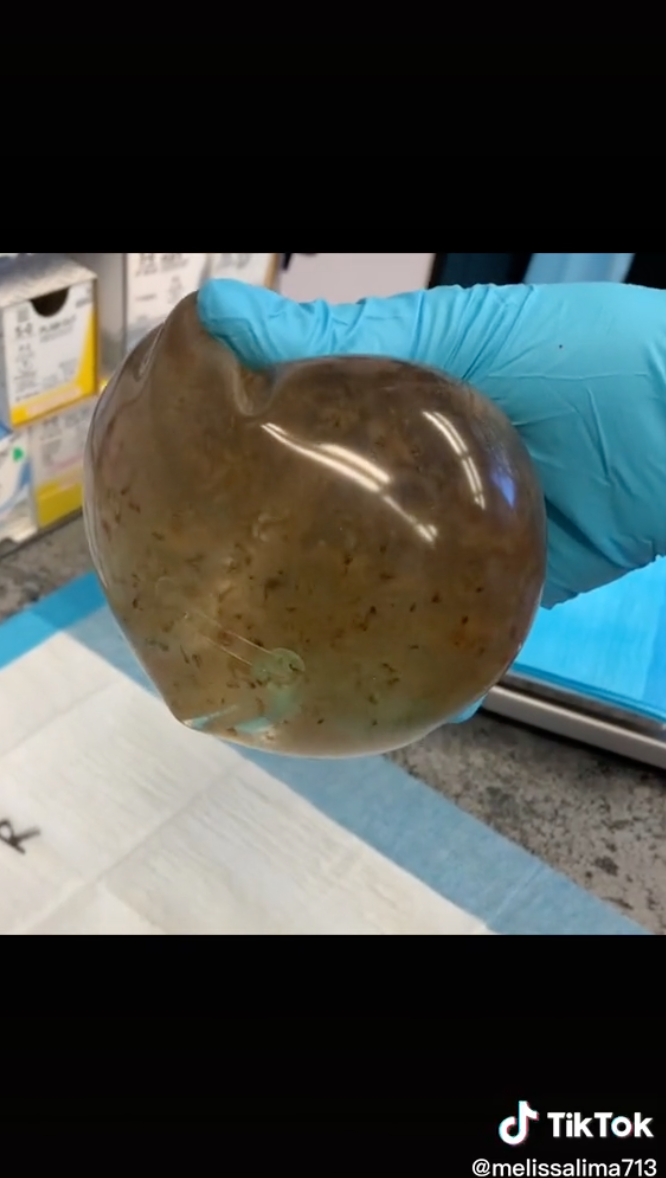
And her doctor had no idea how the mold grew and told he had "never seen that before."
Within hours of having her breast implants out, Melissa started to feel better.

And now, two years later, Melissa said she is about 90% better. "I still have to take medication for Hashimoto's and I have joint pain in my hips. Other than that, I'm happy, healthy, and more importantly, extremely lucky to be able to get back to my normal self," she said.

Melissa said she's not trying to tell people not to get implants, just that it's a good idea to research breast implant illness and be mindful of symptoms. "I know most surgeons will tell you that they're 'safe,' but you never know how they will react inside of your body."

To get more information about breast implant illness and breast implants in general, BuzzFeed also spoke to Dr. Joshua Lampert, FACS, who has been practicing for 12 years. He is a plastic, reconstructive, and aesthetic surgery diplomate and a member of the American Board of Plastic Surgery and the American Society of Plastic Surgeons.
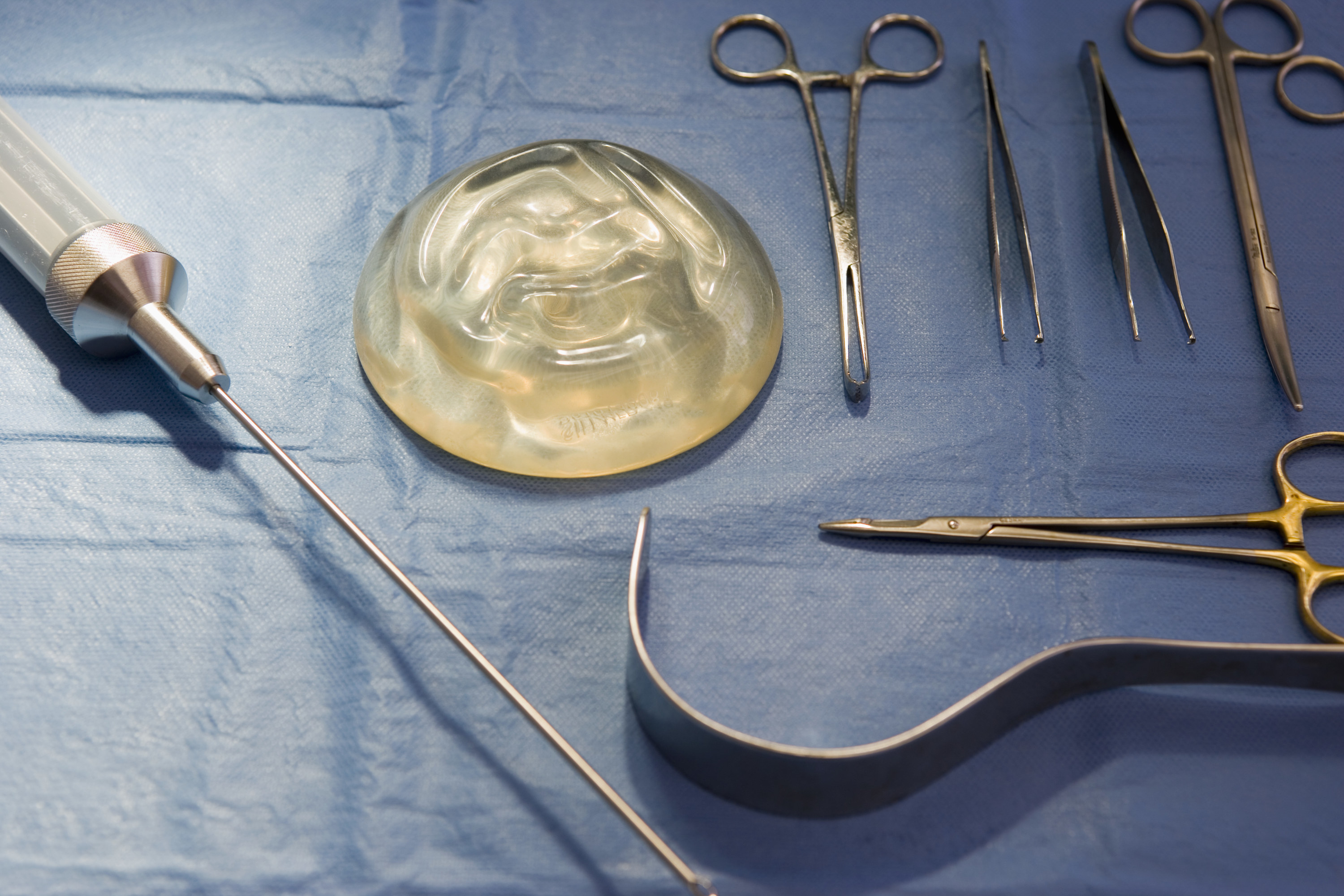
Currently, there are two different types of breast implant options: silicone and saline. "In the USA, there are a variety of both saline and silicone breast implant options. Of the silicone implants, there are varieties of thicknesses or 'cohesive' silicone gels. The thickest of which resembles more of a 'gummy bear' consistency with a thicker gel filling."

Dr. Lampert confirmed that the current breast implant options on the market today are all equally safe, according to safety studies.
"Some things to be aware of, though: When a saline implant ruptures, your body absorbs the saline. When a silicone implant ruptures, the silicone can either be contained within the scar capsule or spread outside the capsule through tissues and to the lymphatic and lymph nodes. Some people have hypothesized that silicone is more dangerous for this reason, but to my knowledge, no large level I-II evidence-based studies exist to support this," he said.
Dr. Lampert also had some facts about saline implants. "Saline implants must be filled by the surgeon. If there is contamination (even from the ambient air in the operating room), things like this fungus can occur inside the implant over time. Some people have hypothesized that saline is more dangerous for this reason, but to my knowledge, no large level I-II evidence-based studies exist to support this. Many of us agree now that textured implants are more dangerous due to their association with BIA-ALCL, a cancer of the immune system. I do not know anyone in the US who still uses them."
In addition, breast implant placement and removal with a board-certified plastic surgeon through the American Board of Plastic Surgery should be extremely safe, Dr. Lampert said. "Of course, this should be performed with a board-certified anesthesiologist providing anesthesia, a registered nurse (RN) with the patient in the operating room, and recovery. These surgeries should also be performed in an AHCA-licensed or appropriately accredited surgical facility. One cannot cut corners on safety."
"Implant-based breast augmentation was the most popular cosmetic procedure performed by members of the American Society of Plastic Surgeons in 2018, according to the National Plastic Surgery Statistics. From 2005 to 2018, more than 3 million breast implants were placed in the United States and Canada. More than 1.8 million breast augmentations were reported worldwide in 2018 by the International Society of Aesthetic Plastic Surgery. Although breast augmentation has well reported high percentages of patient satisfaction, breast implants are associated with a significant rate of local complication reoperation. An estimated 20% of patients develop problems or complications related to the procedure, including capsular contracture, rippling and wrinkling, implant displacement, asymmetry, late hematomas, and neoplasm," Dr. Lampert said.
Patients may lose nipple sensation and the ability to breastfeed after getting breast implants. "This can happen with any breast surgery but is of higher risk with breast lifting or any scar around the areola. Breast implants can also rupture. Silicone gel breast prosthesis rupture rates have been reported between 8.7 to 24.2% at 10 years."
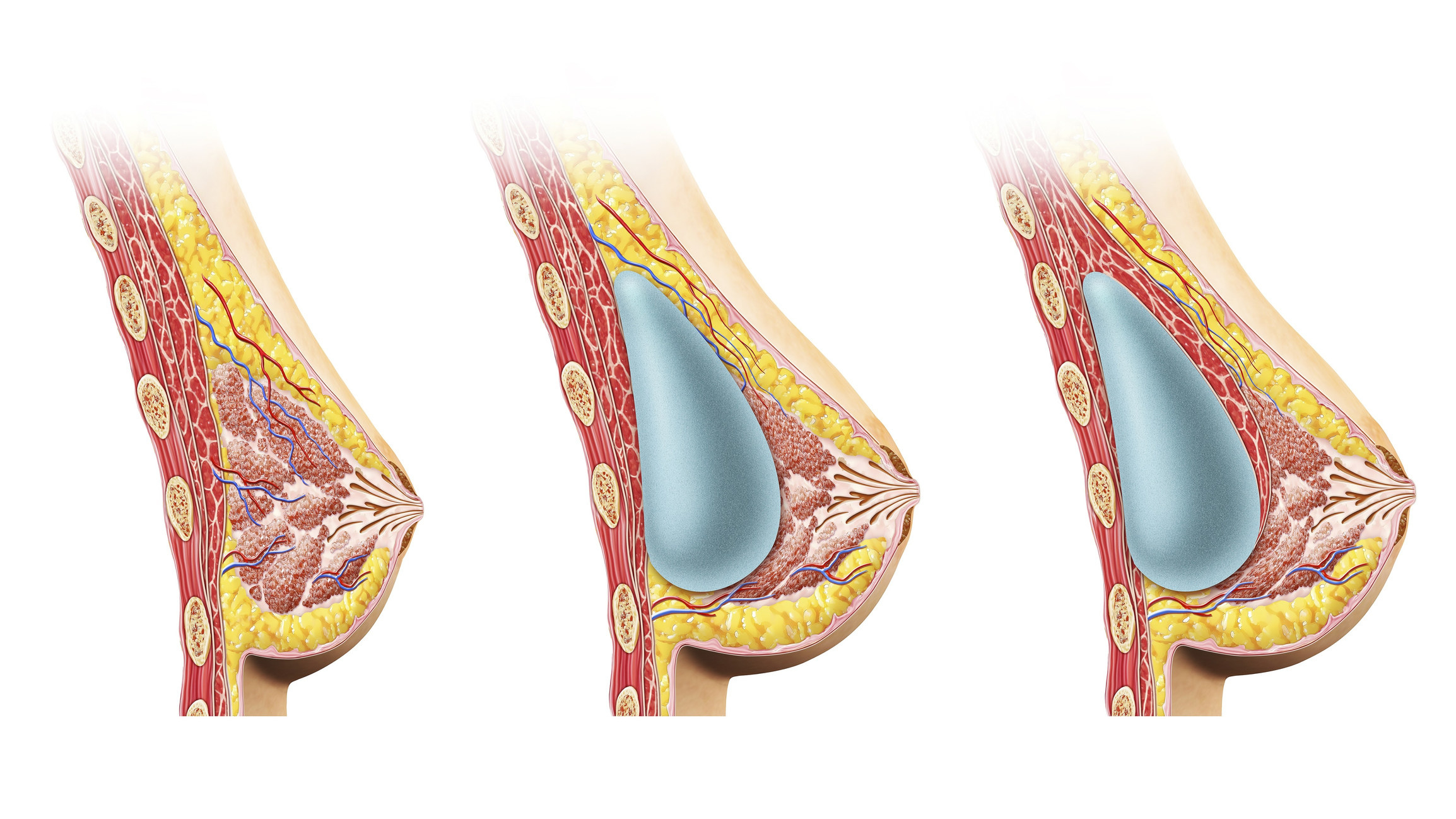
Dr. Lampert said that all breast implants will need to be removed or replaced eventually — typically due to capsular contracture, or scar tissue that develops around the implant. "Capsular contracture is not really an unexpected complication from breast implants. With enough time, we expect capsular contracture to occur to some degree in the majority of patients. The natural evolution we anticipate is that the body will encapsulate the breast implant in the scar. This is called the capsule. The capsules thicken and tighten over time, which is also known as capsular contracture."
When it comes to breast implant illness, Dr. Lampert has been spreading awareness on his social media platforms. "Common symptoms patients with BII complain of include inflammation of various parts of the body, hair loss or alopecia, memory and concentration problems (or 'brain fog'), muscle and joint pain, rashes, anxiety, shortness of breath, insomnia, visual disturbances and impaired vision, gastrointestinal issues, dry mouth, dry eyes, depression, headaches, and fatigue."
Dr. Lampert also added that BII is really just now being better recognized and further accepted in the mainstream scientific community, but reports of autoimmune disease with breast implants were published back in the 1990s. And even with all of this evidence, there sadly are many doctors who still don't believe in BII.
"When I started doing a lot of explants around nine years ago, I was not so sure BII existed myself. I had a large breast implant revision practice and inevitably a lot of patients decide to remove their implants eventually for a number of reasons (pain, rupture, BII, etc.). Once a person decides to remove her implants, my approach is always to support, discuss options, set expectations, and educate with photos of similar patients. Over time, I saw so many patients tell me that their BII symptoms improved once the implants came out. I saw explant patients with abnormal autoimmune panels improve after removal. I saw rheumatoid arthritis get better. I saw rashes go away. I saw low platelets rise. I saw multiple patients regain normal menstrual cycles and get pregnant. I saw so many patients get better that it is impossible for me not to believe in BII."

Breast implant illness can occur in patients with any type of implant and there is currently no way to determine if you are at higher risk of developing BII prior to getting implants. "Practicing on a diverse patient population here in Miami, BII seems to happen with equal occurrence to all ethnic and all age groups. I have had patients who have acquired it within months or within decades after getting their implants. If you have any pre-existing autoimmune disease or prior history of questionable autoimmune illness, it may be wise to speak to a rheumatologist prior to deciding on surgery," Dr. Lampert said.
In addition, no one really knows how common breast implant illness is. "The FDA has been looking into it more deeply since 2019. I think, over time, it is more common than we think. So many breast implants are placed every year, that even if only a few percent acquire BII per year, it becomes a lot of patients and is no longer a rare disease," he said.
Special thanks to both Melissa and Dr. Lampert for generating important conversations around breast implants.