
Last May, when she was 10 weeks pregnant, Eunice Lee took a blood test to screen for diseases in her baby.
The test, called MaterniT21 PLUS, promised clear answers about the sex of her fetus as well an array of disorders, including Down syndrome. At 40 years old, Lee knew her baby had an elevated risk of genetic disease, and so she wanted this information as soon as possible.
Two weeks later Lee went to her obstetrician's office to get the results. But instead of hearing about her baby's genome, she got a shock about her own health.
"My OB walked into my room and was holding the sheet of paper in her hand," Lee, an anesthesiologist in Santa Barbara, California, told BuzzFeed News. The doctor had just hung up the phone with Sequenom Laboratories, the San Diego company that performs the test.
"The director of the laboratory called my obstetrician and told her I needed to be worked up for cancer," Lee said, "which was just alarming, to her and also to myself, because I had no idea I had cancer."
MaterniT21 PLUS was the first noninvasive prenatal test (NIPT) to hit the market, in October 2011, and Sequenom has sold more than 400,000 of them. Five other companies — three in California and two in China — sell similar tests, and demand is rising sharply.
"There's been about 800,000 women in the past year in the U.S. who have had an NIPT," Eric Topol, a professor of genomics at the Scripps Research Institute, told BuzzFeed News. That's a lot — about 20% of the 4 million total babies born each year. "It's the hottest molecular test ever in the history of medicine."
As the numbers tick upward, these tests — which only require a blood draw — are turning up rare genetic glitches not only in the DNA of the fetus, but the mother.
Today at the Future of Genomic Medicine conference in La Jolla, California, scientists from Sequenom said they have seen more than 40 cases in which the test revealed an abnormal genetic profile suggestive of cancer in the mother. At least 26 of these women were subsequently confirmed to have cancer, including Eunice Lee.
Because these popular tests are largely unregulated by the Food and Drug Administration (FDA), the companies are struggling with how to handle these sticky situations. The tests were not designed to detect cancer, and no one knows how often they are wrong when used for this purpose. And yet, withholding this potentially life-saving information from women might also cause harm.
"No company, no doctor, no patient ever expected this," Topol said. "This is going to happen to many other women going forward."
It also hints at a not-so-distant future in which people routinely get blood tests for cancer, known among scientists as "liquid biopsies." At least two of the companies that sell these prenatal tests have announced plans to enter the oncology market.
"It makes you wonder where this is all going," Topol said, "and not just among pregnant women."
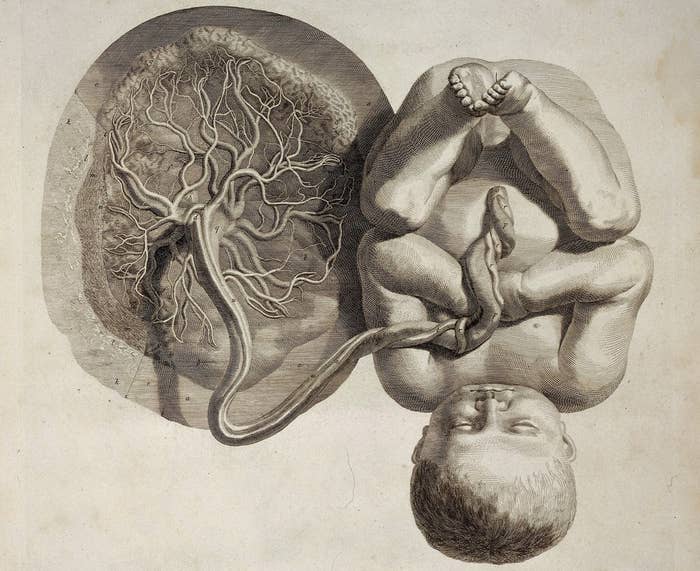
The tests look at bits of fetal DNA that float in a pregnant woman's blood. During the normal course of fetal development, some cells of the placenta die and release fragments of the baby's DNA into the mother's bloodstream.
On average, about 10% of a pregnant woman's circulating DNA comes from her fetus. "It's quite substantial," Dirk van den Boom, chief scientific and chief strategy officer at Sequenom, told BuzzFeed News.
The MaterniT21 PLUS test focuses mainly on chromosomes 13, 18, and 21 because of their links to well-known genetic diseases. Whereas people usually carry two copies of each chromosome, a fetus with three copies of chromosome 21 will develop Down syndrome.
The test doesn't distinguish which DNA pieces are maternal and which are fetal. Any extra or missing chromosomes it finds are assumed to come from the baby, because an adult woman carrying them would most likely be infertile. "We work from the assumption that a pregnant woman is considered normal," van den Boom said.
But sometimes she's not. If she has cancer, for example, then tumor cells may leak their DNA — lousy with chromosomal defects — into the bloodstream. When MaterniT21 PLUS finds these unusual signatures, the test result comes back as "non-reportable," meaning that it cannot determine whether the fetus has a chromosomal disease.
A non-reportable test result can have many possible explanations. "There are all kinds of kooky things that you find," Diana Bianchi, professor of obstetrics and gynecology at Tufts University School of Medicine, told BuzzFeed News. Bianchi is a consultant for Illumina, a large San Diego biotech that sells prenatal tests.
For example, in an Illumina-funded study published last month, Bianchi and her colleagues described a pregnant woman whose prenatal test found bits of Y chromosome in her blood and predicted that her baby would be a boy. Instead, she had a girl. As it turned out, the Y chromosome had come from the woman's kidney, which years earlier had been transplanted from a male donor.
In 2013, scientists reported a case of a prenatal test detecting cancer in a pregnant woman, a 37-year-old who had vaginal cancer. But Sequenom's announcement today offers the first large set of numbers.
Sequenom's tests have discovered several types of cancer, both malignant and benign, including cancer of the breast, colon, and uterus, the company reported.
Doctors deal with these so-called "incidental findings" all the time, Robert Green, a medical geneticist at Brigham and Women's Hospital in Boston, told BuzzFeed News. "This is part and parcel of the practice of medicine." A CAT scan you get after banging your head, for example, might spot a hidden tumor.
When it comes to prenatal tests, however, it's not clear whether incidental findings have clear-cut diagnostic value. It will be crucial to know not only how many times they successfully detected a pregnant woman's cancer, but how often a suspicious result turned out not to be cancer, Green said.
Otherwise, he added, the test might spur a woman to go through unnecessary medical procedures. "The question is, how much cost, pain, radiation, and surgery might take place for a false positive?"

Prenatal tests have been the source of much controversy over the last few months, particularly after The New England Center for Investigative Reporting published a story about women who got abortions based on their test results, only to find out that the tests were wrong.
"How this works out in practice is that we're constantly finding things that might mean something but we're not 100% sure," Laura Hercher, a genetic counselor at Sarah Lawrence College, told BuzzFeed News. "It's led to some unfortunate outcomes."
Because these tests are developed and used in a single laboratory, they do not have to go through an FDA approval process before going to market. The agency has offered little guidance about how to deal with incidental findings.
"The FDA is struggling to figure out how to regulate these things," Hercher said. "Everybody's screaming and yelling about what it's going to look like."
The FDA's inaction means that companies don't know what to do with prenatal test results that relate to the mother's health. "It's a funny spot for the lab to be in," Hercher said. By giving the women the inconclusive cancer findings, she added, the lab could be inviting regulatory sanctions.
On the other hand, if they didn't release the results, that could cause the women harm. "It's really hard, ethically, to make the case that you should sit on this information," Hercher said.
Sequenom said that in these rare cases it emphasizes to the women's doctors that its test is not a validated cancer screen. "You accumulate enough experience over the years that you can say these profiles are suggestive of a disease," said van den Boom of Sequenom. "You can't tell for sure but it's information you can report back to the physician."
Meanwhile, the company is using what it has learned from these rare cases to help develop new tests specifically for cancer, van den Boom said. "We're getting a glimpse of what the technology can do."
BuzzFeed News reached out to the other three American companies that sell noninvasive prenatal tests to ask whether their tests have also detected cancer in pregnant women. Illumina declined to comment. Ariosa Diagnostics did not directly answer the question, but said that its test had only been validated for prenatal indications.
The third company, Natera, said that it doesn't have this problem because its test looks at individual letters in the genome, rather than whole chromosomes.
Natera, like Sequenom, is eager to move into oncology. "It's obvious to see what incredible benefit it would be if we could accurately sample someone's blood and identify [tumor] DNA," Sue Gross, the company's chief medical officer, told BuzzFeed News. "It would be groundbreaking."

After her obstetrician told her about the possibility of cancer, Eunice Lee called Sequenom's laboratory director, Nilesh Dharajiya, to find out more about her test results.
Dharajiya emphasized that MaterniT21 PLUS had not been designed to diagnose cancer, and that no one knew yet how accurate it was. Still, the test had detected cancer in a small number of women. "He thought it would be in my best interest to get a full-body MRI to try to find out whether I indeed had a malignancy," Lee said.
So she did, and the scan found a 7-centimeter tumor in her colon. That very evening she had the tumor removed with laparoscopic surgery. The surgeon also took out 49 lymph nodes, which all turned out to be benign.
Lee learned that about 86% of people with her type of colon cancer are cured with surgery alone. So she decided not to do additional chemotherapy for the rest of her pregnancy. On Nov. 24, she delivered a healthy baby boy, Benjamin. She hasn't had any symptoms since.
"I just felt like I was the luckiest person in the world," Lee said. "In my case, the test probably saved my life."
As a doctor herself, Lee fully understands that a prenatal test is not a definitive screen for cancer. Even so, she was eager to find out whatever information it could provide.
In fact, after her surgery, when she was seven months pregnant, Lee took the MaterniT21 PLUS test a second time — not to find anything about her baby, but to see whether it would still pick up any circulating tumor DNA in her blood. (It didn't.) "It was purely on my own initiative," she said. "It was for my peace of mind."
Based partly on this second prenatal test result, as well as a follow-up MRI and discussions with her oncologist, Lee has decided not to pursue any further cancer treatment. "I hope I made the right decision."
