People Tell Us Their Positive Experiences With Clinical Trials
Clinical trials helped these patients better manage their inflammatory bowel diseases (IBD).
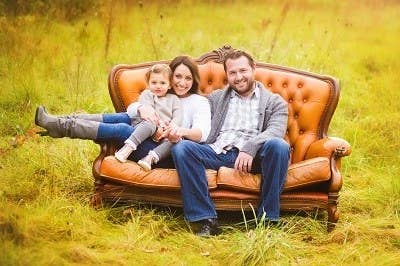
A Mother Gives Life and Learnings

"From a young age, I knew that I wanted to be a mother. But, when I began experiencing symptoms of Crohn’s disease at age 21, I became worried about how my future may look. ... Research into the topic wasn’t as plentiful as I would have liked, and the message boards and mom blogs were full of more questions than answers. As it would turn out, I would need to participate in the research if I wanted to help answer this question.
"Once on proper medication and in confirmed remission, my husband and I got happy news: We were expecting. After congratulating us, my doctor brought up the possibility of taking part in a pregnancy study. ... Throughout my first pregnancy, I would chat on the phone with the research coordinator, who asked questions about disease activity, medication use, infections, and overall health. [Later] I would answer questions about my health and breastfeeding status, as well as [my son's] overall health. ... It was such an important topic of research that I was happy to start the process all over again when, almost two years later, I became pregnant a second time.
"Both of my sons and I have taken part in this study since 2012, and it’s one of my proudest contributions to future moms who are faced with a hard decision, just as I was: Is it safe for me to take my IBD medications while pregnant? Now that some of the results are being shared across the world, it’s amazing to know that moms will now have more information at their fingertips. Contributing to research doesn’t always mean signing up for the latest drug trials. It may mean tackling an area of disease management that is not currently well researched and contributing your experiences to further the medical community’s understanding of it."
—Jessica
Returning to Everyday Life

"I was diagnosed with mild ulcerative colitis in early 2010. Though I took the prescribed medications, the UC was continuous and worsened over the next three years until I had exhausted all approved treatments to no avail. A specialist ... recommended I consider a clinical trial medication as a potential treatment. I was screened and accepted for the clinical trial. My UC was then moderate and affecting my daily work and activities, so I was hopeful.
"My doctor and his clinical trial nursing staff were great — friendly, communicative, honest, professional, and organized. I visited them every three months for required blood draws, general health review, written clinical trial status paperwork, and replenishment of the medication. There was also a convenient simple daily phone report for seven days prior to my quarterly visits and an annual flex sigmoidoscopy or colonoscopy for visual evidence of the effects of the medication on my colon healing.
"I am so grateful that the medication was effective, over a reasonable time period, in reducing my UC symptoms and has now essentially healed my condition with minimal side effects, as I remain on the clinical trial medication. My lifestyle and activities are back to normal. The time involved in the clinical trial program has been well worth it. I consider the clinical trial staff my friends and hope the medication will benefit others when it is approved for general prescription."
—Michael
A Successful Last Resort After Failed Surgeries
"The trial I found most interesting was a study on the efficacy of a stem cell procedure being performed in Madrid, Spain. The two leading doctors behind the study had excellent credentials. ... I emailed them explaining my condition [(perianal abscesses that manifested into an intersphincteric fistula and failed ileostomy)], my research on their trial, and my eagerness to fly to Spain for treatment and almost instantly received a response back. ... After a few weeks of back and forth, I was accepted as a patient. However, since only European Union citizens technically qualify for the study, I would have to pay cash to receive the treatment.
"When I arrived in Spain, I was to have liposuction performed to extract the adipose tissue to collect cells for replication. ... I woke up to my stem cell surgeon running over in excitement! He was holding a small vial containing the 5 million stem cells collected. ... I was relieved that we had been able to culture the cells successfully. It was truly a special moment. A few hours after the liposuction, the surgeons injected 4 million stem cells into the branch fistula and 1 million into the main trunk.
"Eight weeks later, I was back home in the USA. ... With results from my MRI taken earlier in the day, [my GI and surgeon] concluded that the results revealed a closed fistula at the branch — the stem cell treatment worked! I went back to Spain in April 2017 for my second treatment, which consisted of placing about 45 million cells into the remaining fistula. ... Finally, in July, it was concluded that my fistulas were officially healed! This result gave me the opportunity to get my ileostomy removed on Nov. 8, and I haven't looked back since."
—Brandon
Gaining Acceptance

"When I was diagnosed with ulcerative colitis as a 20-year-old, I never thought I would go so far as enrolling in a clinical trial to manage my disease. I was actually very resistant to most medications in the beginning. It’s hard to come to terms with being dependent on medication for the rest of your life when you are supposed to be in your prime. ... Over the next four years, I tried several medications but only saw a wink of improvement in my disease.
"Enrolling in a clinical trial for a new drug is intimidating. There is lengthy paperwork, and the wording may cause even more apprehension. The screening processes usually require an extensive wash-out period, which might cause your disease to worsen. I actually missed out on one drug trial because it suddenly closed enrollment during my wash-out period. But, despite these downfalls, clinical trials serve as 'end of the rope' strategies to manage disease in patients who don’t respond to standard of care options.
"So, in late 2017, I signed the paperwork and started my journey as a clinical trial patient. After so many failures, I have learned to practice cautious optimism when trying new medications. Just a few weeks into the open-label trial (this just means my doctor and I both know that I am not getting placebo), I began to see positive changes in my disease. Now a few months into the trial, I am feeling energetic again, I am not worried about finding a restroom urgently, and my symptoms continue to improve. It seems that for the first time since my diagnosis, I may be approaching remission."
—Paige
