Birth control is not one-size-fits-all. It's not even one-size-fits-most.

BuzzFeed Health teamed up with a board-certified gynecologist to create a guide that helps you decide which birth control is right for you.
BUT we're not going to tell you exactly what to use — sorry, we're journalists, not your doctor. That decision will likely be based on not just your health and lifestyle but your insurance coverage and access to certain methods. What we can do is tell you exactly what questions to ask your doctor so that you can make an informed decision about your birth control.

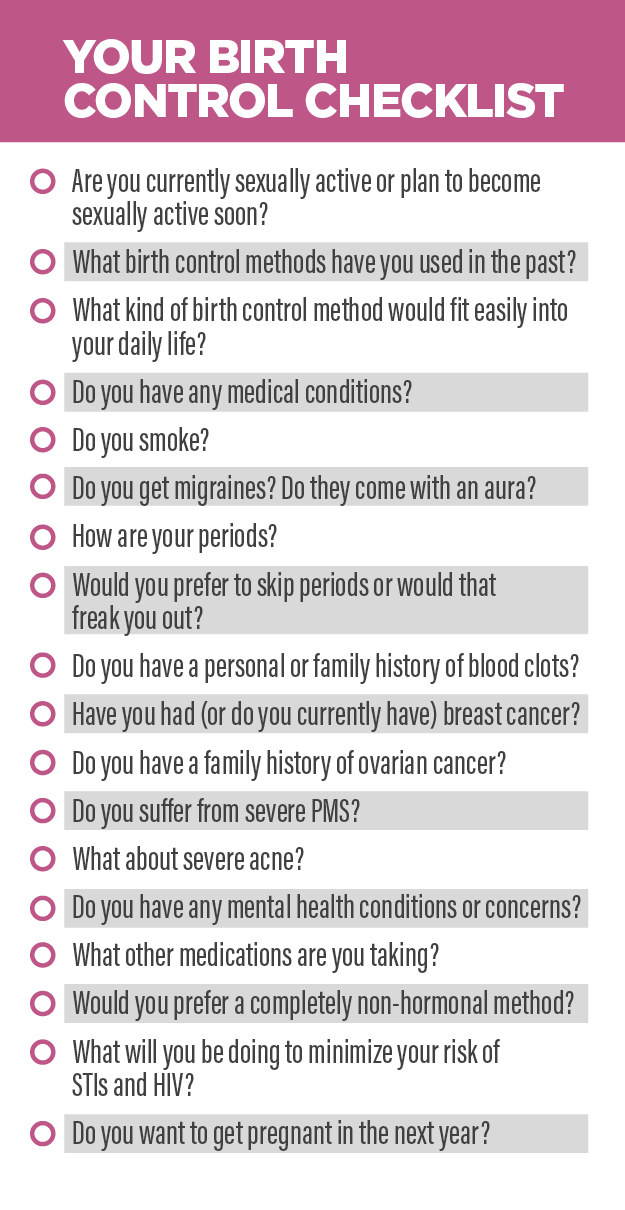
1. Are you currently sexually active, or do you plan to become sexually active soon?
2. What birth control methods have you used in the past?
3. What kind of birth control method would fit easily into your daily life?
4. Do you have any medical conditions?
5. Do you smoke?
6. Do you get migraines? Do they come with an aura?
7. How are your periods?
8. Would you prefer to skip periods or would that completely freak you out?
9. Do you have a personal or family history of blood clots?
10. Have you had (or do you currently have) breast cancer?

11. Do you have a family history of ovarian cancer?
12. Do you suffer from severe PMS?
13. What about severe acne?
14. Do you have any mental health conditions or concerns?

15. What other medications are you taking?
16. Would you prefer a completely non-hormonal method?

17. What will you be doing to minimize your risk of STIs and HIV?

18. Do you want to get pregnant sometime in the next year?
Got all that?