A few years ago, I found out that the results of my annual Pap smear came back "positive." A Pap smear is a procedure performed by a gynecologist to screen a patient for cervical cancer. If the test comes back positive, it means that abnormal or unusual cells were found on the patient's cervix. This doesn't automatically indicate cancer, but a closer look is often needed to make sure these cells aren't progressing toward cancer.

Thankfully, I was educated about abnormal Pap smears and knew I shouldn't immediately go to a bad head space. Many of my friends who were sexually active had also had positive Pap tests in the past, and they reassured me that a dire outcome was unlikely. In fact, a 2004 study that sampled 11,739 women found that 20% of them reported at least one abnormal Pap smear in their lifetime. And according to the Roswell Park Comprehensive Cancer Center, less than 1% of women with positive Pap tests are diagnosed with cervical cancer.
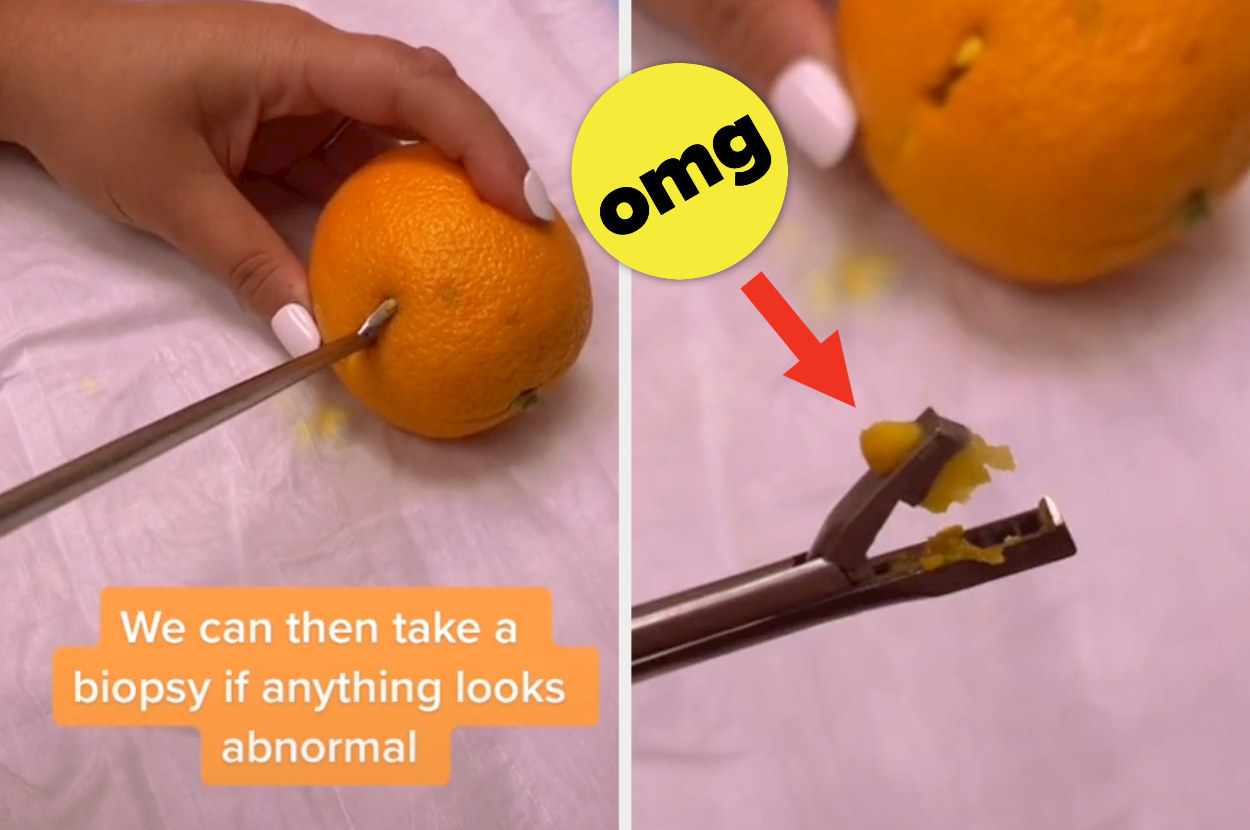
After I was notified about my positive Pap test, my doctor told me to get another smear in three months. If the abnormal cells were still present, I would need to get a colposcopy. A colposcopy is a procedure where a doctor uses something called a "colposcope" to closely examine your cervix, vagina, and vulva for signs of disease. Sometimes during the procedure, they'll biopsy parts of your cervix or vagina for laboratory testing.

Sure enough, my results came back positive, so a colposcopy was in order. But this time, I was definitely a little freaked out. Not because I was scared of the outcome — my OB-GYN had reassured me that this was just an extra screening precaution and I most likely did not have cancer. I was scared because my friends who had colposcopies before said they hurt like a BITCH. "It was the most painful thing I've ever experienced," one of them told me, quite bluntly.
On the other hand, my mom had one before, too, and said it wasn't painful for her. So the day of the procedure, I tried my best to go in with an open mind. When my gynecologist started to tell me what to expect, she said I might experience some "discomfort," but no "pain." The distinction between those two things has always been a bit blurry for me, so her words weren't necessarily comforting. She also said the outer part of the cervix didn't have nerve endings, so that's why I wouldn't feel pain.
Let's just say...I wish I didn't remember my colposcopy as clearly as I do. For those who are unaware, a speculum is an instrument they put up your vagina to keep it open for examination. That alone caused a lot of pain for me, since I'm usually desperate for them to take it out after a few seconds during my yearly exam. But nope, it's in there the entire 20-minute procedure. On top of the agony of having a foreign metal object inside of me, I could feel her poking and prodding around my cervix and vaginal wall. And even though she said my cervix didn't have nerve endings, I definitely felt a lot of pressure in the two spots that she biopsied. It didn't help that whenever I yelped in pain, my doctor said, "I don't know why you're yelling; this doesn't hurt." That reminds me — I really need a new fucking gynecologist.
I then realized that my cervix was literally HOLE PUNCHED.
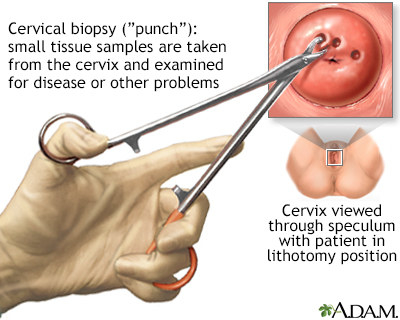
Here's an official diagram, so that you know this isn't a joke:
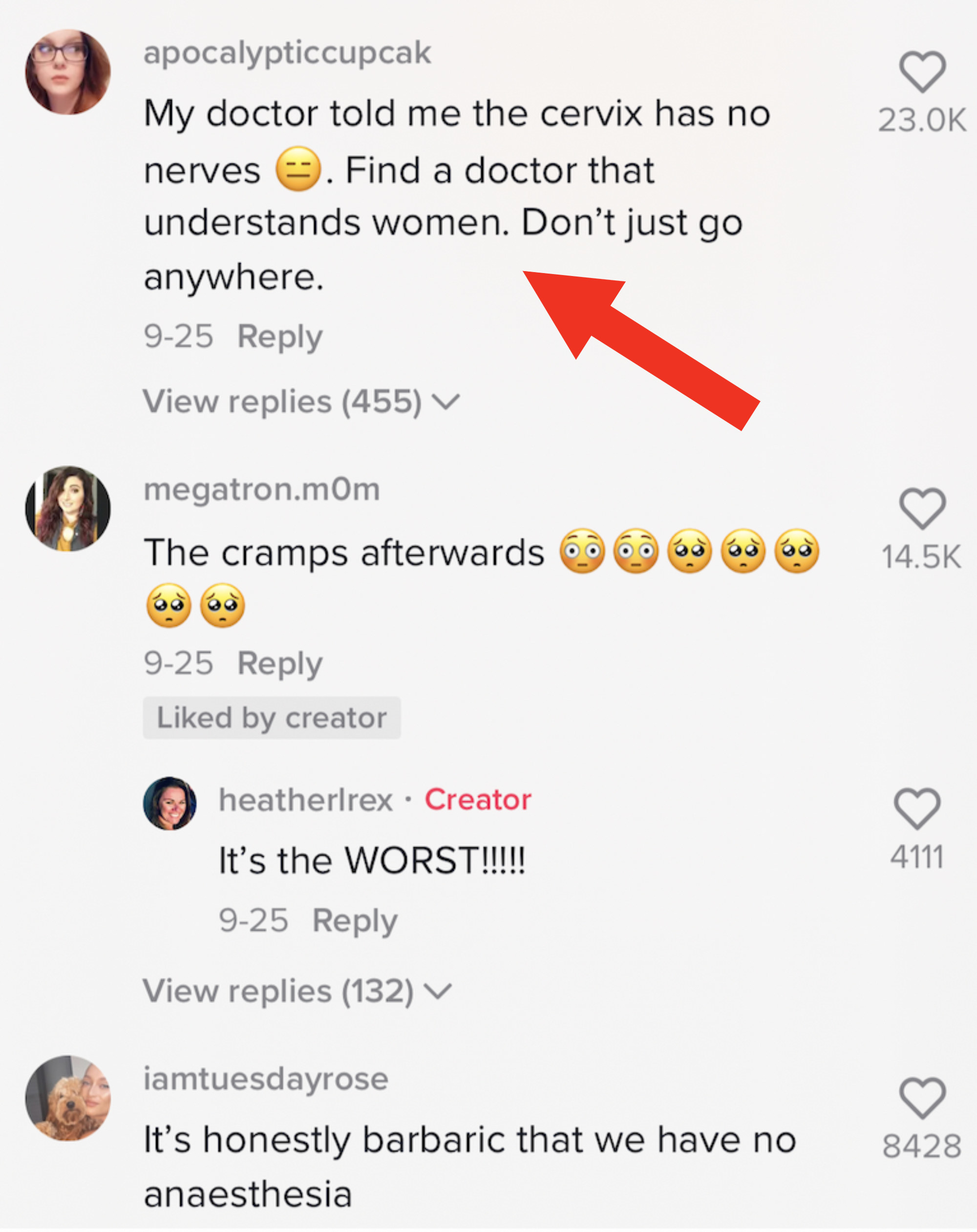
The comment section of the video was even more horrifying, because it was filled with people sharing their traumatizing colposcopy experiences — some of which were eerily similar to my own.
These stories combined with my own experience had me wondering whether there was a reason we weren't receiving anesthetic for such a common procedure, or if this simply came down to the age-old issue of medical workers failing to prioritize women's pain. I decided to reach out to Dr. Diane J. Horvath — an OB-GYN in Baltimore, Maryland — to help tie up some of these loose ends.

My first question was about the logistics of the biopsy — did they really take out a full chunk like that? "The tools used to get biopsies are called cervical biopsy forceps. Most healthcare providers use one that is quite a bit smaller than the one in the video, and creates a biopsy specimen that's about the size of the tip of a pencil (2–3 millimeters)," Dr. Horvath told BuzzFeed. "I'd say that the video significantly overestimates the size and depth of the average biopsy."
But even if the "chunks" they took out weren't as big as in the video, why were so many people still experiencing extreme pain during these procedures? "Everybody's bodies are different, and the way we experience pain depends on our nerve structure, our past experiences with medical care, past experiences with pain, certain medications we are taking, and cultural/societal expectations about pain," Dr. Horvath said. "People's expectations can vary as well — someone who is told they will feel cramps might be surprised when they're not as bad as they imagined they would be, while someone who is told 'you won't feel any pain' might be surprised by even mild cramping that they weren't expecting to have."
When I asked her about whether there was truth to my doctor's claim that the cervix "had no nerve endings," she said, "While it is true that the outer part of the cervix (the area that is typically biopsied during a colposcopy) has fewer nerve endings than other parts of the reproductive tract, there are definitely still nerves that can send pain signals back to our brains and register pain and discomfort. Some people feel literally nothing during a biopsy, while other people feel an intense cramp or pinch. Also, just the experience of having a speculum inside the vagina can be painful for some people."
Even though my OB-GYN didn't offer me any pain management solutions, I was curious as to whether this was something other doctors implemented. "Most healthcare providers recommend that people take oral pain medication like ibuprofen or naproxen before their colposcopy, which can help with the crampy pain some people have during and after the procedure. We can also offer a topical anesthetic (like a gel applied to the cervix) or a local anesthetic that is injected with a small needle (which unfortunately can also cause pain). For people with severe pain, anxiety, or a history of trauma that makes it hard to undergo exams and procedures, I've done colposcopies using IV sedation," Dr. Horvath said.

