A survey of 640 GPs from five major Australian cities has discovered most doctors support the prescription of medical cannabis and think it's a safer route than opioids or benzos. Yet they feel they don't know enough about it to confidently prescribe it to patients.
Research from Sydney University's The Lambert Initiative for Cannabinoid Therapeutics was published in the British Medical Journal Open on Wednesday. It's the first study to examine the attitude Australian GPs have towards medical cannabis.
Of the 640 GPs surveyed from August to November last year, 61.5% reported at least one patient asking about medical cannabis in the previous three months, while only 28.8% felt comfortable discussing the drug with patients.
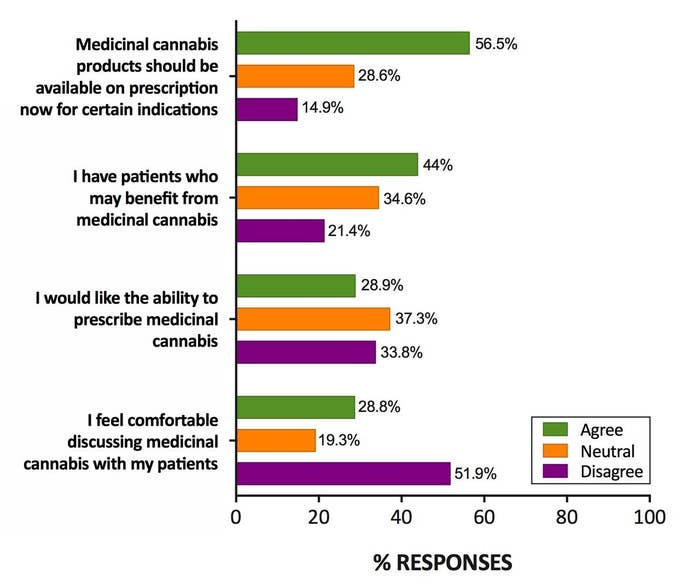
In a damning indictment of the current state of access to medical cannabis for the public, 65.4% "strongly disagreed" that they knew how to access the drug for patients. Nearly nine in 10 (86%) reported having "poor perceived knowledge" of the drug.
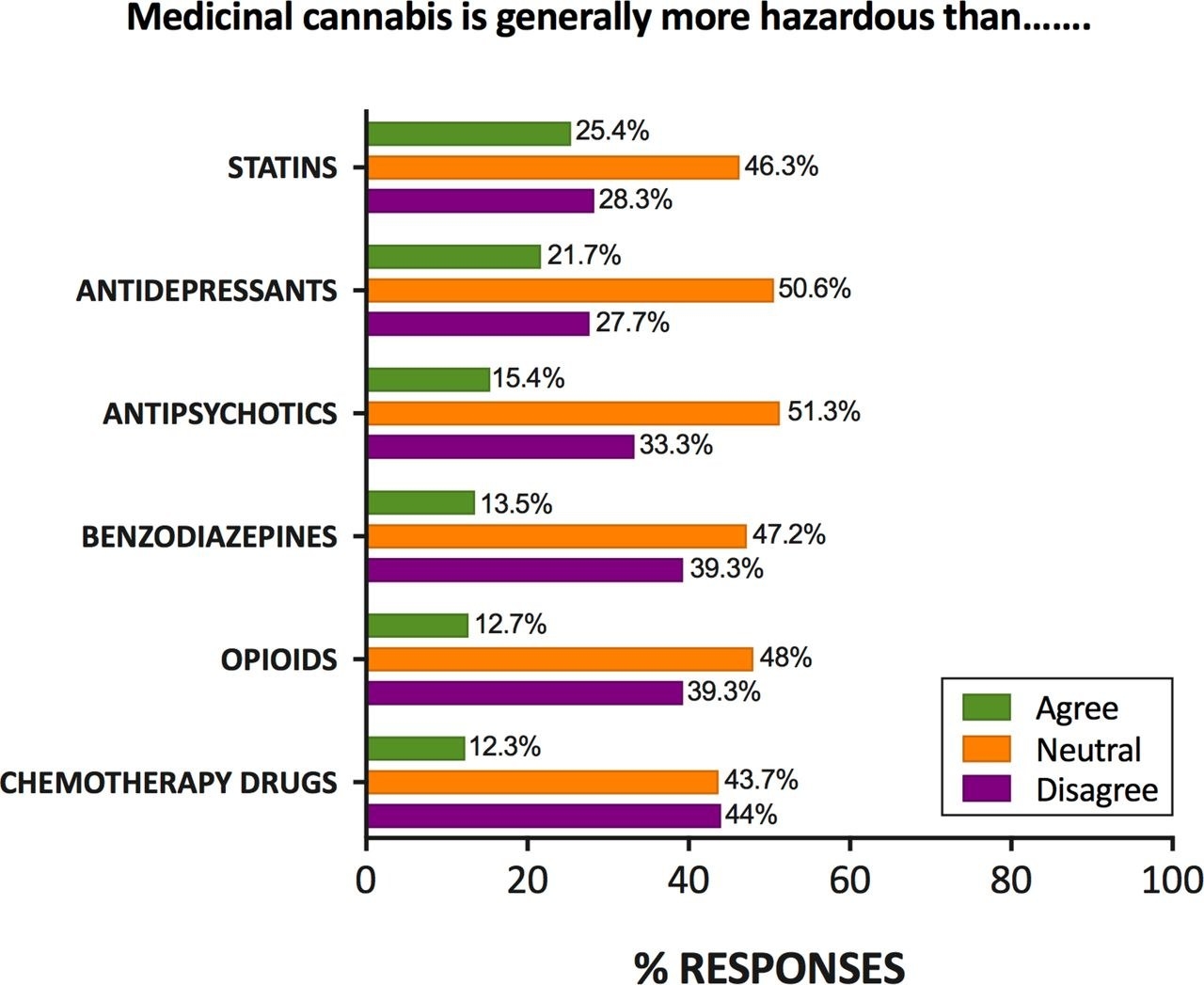
When asked about the danger of medical cannabis compared to other drugs such as opioids, chemotherapy drugs, antipsychotics, and benzos, many GPs believed a medical cannabis route was safer for patients.
Nearly 44% said they were neutral about the comparative hazards of medical cannabis, but of the remaining responses 78% believed medical cannabis was safer than chemo drugs, 75.6% said safer than opioids, and 74.5% safer than benzos.
Research associate at the Lambert Initiative and co-author of the study, Anastasia Suraev, called for a government rethink about the current, specialist-focused prescription model.
"A majority of GPs believe medicinal cannabis should be available by prescription, with the preferred model involving trained GPs being able to prescribe independently of specialists," she said in a statement on Wednesday.
Academic director of the Lambert Initiative (and corresponding author of the study) professor Iain McGregor said GP training and education was "urgently needed", with fewer than 800 patients in Australia having legal access to medical cannabis.
"Part of the problem is the specialist-based model that largely excludes GPs from prescribing," he said. "Most Australians know how hard it is to access specialist medical care, let alone a specialist with an interest in cannabis-based medicine."
The lack of GP knowledge has been known for some time, however this study represents the first time doctors were formally surveyed. The responses echo calls from doctors that have been made multiple times over the last two years. Last year GPs packed a session on cannabis education at the GP17 conference, eager to learn more about the drug and how it is prescribed in the country.
Currently, a GP needs to either become an authorised prescriber for a class of patients or go through the Therapeutic Goods Administration's complicated Special Access Scheme B on a per-patient basis. Typically, GPs will also need to be supported by a specialist to prescribe.
